The Pancreas And Insulin
The pancreas is responsible for producing insulin. The cells which produce insulin are beta cells. These cells are distributed in a cluster of cells in the pancreas called the Islets of Langerhans, named after the anatomist who discovered them
Insulin is a hormone that helps to regulate blood sugar levels by assisting the transport of glucose from the blood into neighbouring cells.
How Does The Human Body Regulate Its Blood Glucose Levels
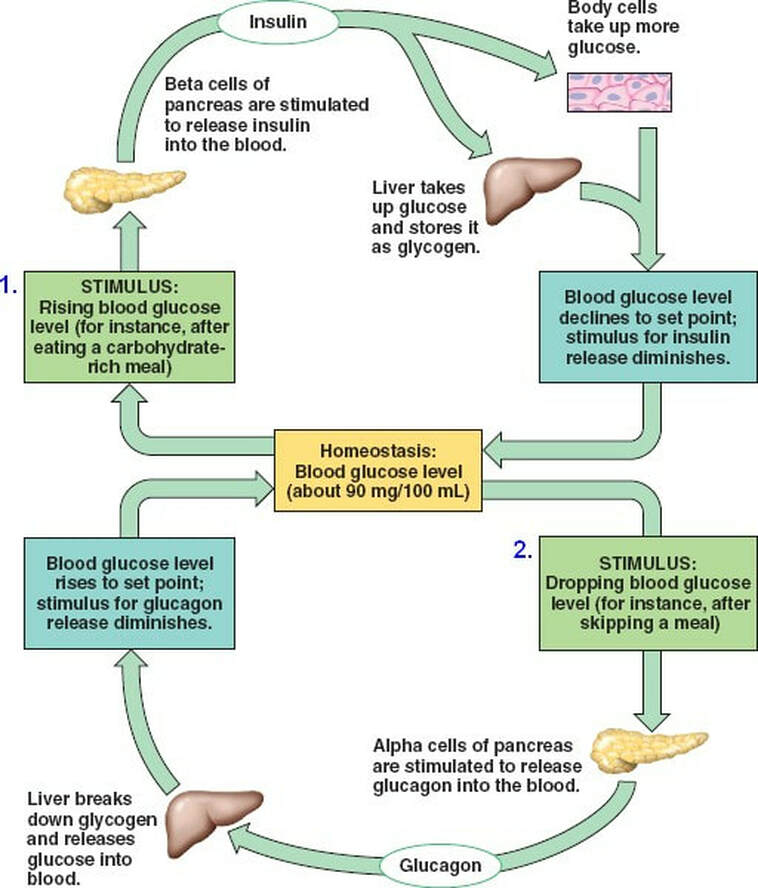
Once a person has eaten a meal, their digestive system will break the nutrients down into smaller components that can travel in the blood to any parts of the body that need them. Any carbohydrates in this food will be broken down into sugars . These sugars will rapidly enter the blood. At this point, it is critical for the body to use the glucose ASAP to avoid hyperglycaemia and maintain a constant blood glucose level. The glucose in the blood is therefore stored in liver and muscle cells in the form of a larger molecule called glycogen. The body is able to detect blood glucose levels via an organ called the pancreas. More specifically, it is detected by areas within the pancreas called islets of Langerhans. In this region there are 2 types of cells. Beta-cells and alpha-cells. Beta-cells will detect high blood glucose and secrete insulin. Insulin is a hormone that will help the liver and muscle cell uptake more glucose and convert it to glycogen, thus lowering the overall blood glucose levels. Alpha-cells will detect low blood glucose and secrete glucagon. Glucagon is also a hormone, but it has the role of breaking down glycogen and releasing glucose from the liver and muscle cells. This will increase the blood glucose. To provide an overview, the components within this system communicate with each other via hormones in order to provide a relatively constant blood glucose level. This maintanence of the internal environment is an example of homeostasis.Continue reading >>
The Role Of The Pancreas In The Body
The pancreas plays a part in two different organ systems, the endocrine system and the exocrine system.
The endocrine system includes all the organs which produce hormones, chemicals which are delivered via the blood to help regulate our mood, growth, metabolism and reproduction.
Two of the hormones produced by the pancreas are insulin and glucagon
The exocrine system is made up of a number of glands which release substances such as sweat , saliva or, in the case of the pancreas, digestive enzymes
You May Like: What Is The Best Blood Sugar Level
How To Stay Healthy In Midlife
As it turns out, the things you do to get a handle on diabetes as you enter midlife arenât that different than what youâve been doing all along to stay healthy:
- Pay attention to your diabetes. That means you need to keep track of your blood sugar levels and talk to your doctor if theyâre are all over the place and you canât figure out why. Keep a record of your results and go over them with your doctor.
- Watch your weight.
- Eat a healthy diet. Get plenty of vegetables, choose whole-grain foods, and opt for lean proteins and low-fat dairy.
- Get at least 30 minutes of exercise a day. It will give you more energy and boost your mood. Youâll get the most benefit by doing a combination of an exercise that ups your heart rate — like brisk walking — along with strength training, like lifting weights.
What Does The Pancreas Do

The pancreas carries out two important roles:
The pancreas produces hormones in its ‘endocrine’ cells. These cells are gathered in clusters known as islets of Langerhans and monitor what is happening in the blood.;They then can release hormones directly into the blood when necessary. In particular, they sense when sugar levels in the blood rise, and as soon as this happens the cells produce hormones, particularly insulin. Insulin then helps the body to lower blood glucose levels and ‘store’ the sugar away in fat, muscle, liver and other body tissues where it can be used for energy when required.
The pancreas is very close to the stomach. As soon as food is eaten, the pancreas releases digestive enzymes into the bowel to break food down. As the food is digested, and nutrient levels in the blood rise, the pancreas produces insulin to help the body store the glucose away. Between meals, the pancreas does not produce insulin and this allows the body to gradually release stores of energy back into the blood as they are needed.;
You May Like: How Long Does Low Blood Sugar Last
Blood Sugar The Hormones And Organs Involved In Blood Sugar Regulation
Welcome to The Nutritional Pearls Podcast! Focusing on topics that include digestion, adrenal fatigue, leaky gut, supplementation, electrolytes, stomach acid, and so much more, The Nutritional Pearls Podcast features Christine Moore, NTP and is hosted by Jimmy Moore, host of the longest running nutritional podcast on the Internet.; Sharing nuggets of wisdom from Christines training as a Nutritional Therapy Practitioner and Jimmys years of podcasting and authoring international bestselling health and nutrition books, they will feature a new topic of interest and fascination in the world of nutritional health each Monday. Listen in today as Christine and Jimmy dig deep into blood sugar regulation in Episode 3.
Heres what Christine and Jimmy talked about in Episode 3:
Beta Cells In Type 2 Diabetes
In type 2 diabetes, the body becomes resistant to its insulin and attempts to compensate by producing a higher quantity of insulin. Research has shown that chronically elevated blood glucose levels over a long period of time can lead to beta cells wearing out, referred to as beta cell turnover or beta burnout.
Scientists are yet to fully understand the exact cause of the failure of beta cells in type 2 diabetes.
They hypothesise that glucotoxicity may be one factor amongst other potential factors including the effects of lipoproteins, leptin and also cytokines, which are active proteins of the bodys immune system.
Read Also: What Happens To Your Body When You Cut Out Sugar
Why Are Hormones Important
Hormones act as chemical messengers that are released into the blood stream to act on an organ in another part of the body. Although hormones reach all parts of the body, only target cells with compatible receptors are equipped to respond. Over 50 hormones have been identified in humans and other vertebrates.
Hormones control or regulate many biological processes and are often produced in exceptionally low amounts within the body. Examples of such processes include:
- blood sugar control ;
- differentiation, growth, and function of reproductive organs and estradiol); and
- body growth and energy production .
Much like a lock and key, many hormones act by binding to receptors that are produced within cells. When a hormone binds to a receptor, the receptor carries out the hormone’s instructions, either by altering the cell’s existing proteins or turning on genes that will build a new protein.;The hormone-receptor complex switches on or switches off specific biological processes in cells, tissues, and organs.
Some examples of hormones include:
Glucose Metabolism And Regulation: Beyond Insulin And Glucagon
You May Like: What Damage Does High Blood Sugar Cause
New Approaches To Drug Development And Therapies With A Particular Focus On Drug Development By Green Synthesis To Cure Blood Glucose Regulation Problems
Bioactive molecules from Natural products have been proved to improve insulin resistance and its associated complications by suppressing inflammatory signaling pathways . Medicinal plants cannot be obsolete and still play a prominent role in human health care. Among natural sources, over 1200 plants have been claimed as antidiabetic remedies. While over 400 plants along with its 700 recipes and compounds have been scientifically evaluated for type-II diabetes. Metformin was developed on the basis of biguanide compound from an antidiabetic herb, French lilac and is now its a first-line drug against type-II diabetes. Medicinal plants also contains a diverse bioactive compounds and can have multiple actions on insulin action, insulin production, or both. With a focus on scientific studies of selected glucose-lowering herbs, phyto compounds and their ability to target insulin resistance, cell function, incretin related pathways and glucose absorption , multiple studies have been done.
Figure 6.
Mechanisms underlying herbal therapies using antidiabetic plants and phytocompounds. Different types of medicinal herbs can be classified based on their modes of action such as insulin resistance , -cell function , and GLP-1 and glucose absorption , The selected.
Regulation Of Blood Glucose
Regulation of glucose in the body is done autonomically and constantly throughout each minute of the day. Normal BG levels should be between 60 and 140 mg/dL in order to supply cells of the body with its required energy. Brain cells dont require insulin to drive glucose into neurons; however, there must still be normal amounts available. Too little glucose, called hypoglycemia, starves cells, and too much glucose creates a sticky, paralyzing effect on cells. Euglycemia, or blood sugar within the normal range, is naturally ideal for the bodys functions. A delicate balance between hormones of the pancreas, intestines, brain, and even adrenals is required to maintain normal BG levels.
Read Also: How To Take Your Blood Sugar
Beta Cells In Type 1 Diabetes
In type 1 diabetes, beta cells die from a misguided attack by the bodys immune system How and why that happens is not clear, but the results of a study published in early 2011 suggest that these pancreatic cells become stressed at the earliest stages of the disease process.
In mice, beta cells respond to this stress by triggering a cell death pathway that results in the loss of beta cell function, and ultimately the loss of beta cell mass.
The study authors from the Indiana University School of Medicine said the exciting findings raise the;possibility that beta cell stress could be part of the trigger for the autoimmune process that leads to type 1 diabetes.
References And Recommended Reading

Ahrén, B. Islet G protein-coupled receptors as potential targets for treatment of type 2 diabetes. Nature Reviews Drug Discovery8, 369385 . doi:10.1038/nrd2782.
Kebede, M. A., Alquier, T., et al. Lipid receptors and islet function: therapeutic implications? Diabetes, Obesity and Metabolism11, 1020 . doi: 10.1111/j.1463-1326.2009.01114.x.
Kim, H., Toyofuku, Y., et al. Serotonin regulates pancreatic beta cell mass during pregnancy. Nature Medicine16, 804808 . doi:10.1038/nm.2173.
Langenberg, C., Pascoe, L., et al. Common genetic variation in the melatonin receptor 1B gene is associated with decreased early-phase insulin response. Diabetologia52, 15371542 . doi: 10.1007/s00125-009-1392-x.
Regard, J. B., Kataoka, H., et al. Probing cell type-specific functions of G in vivo identifies GPCR regulators of insulin secretion. Journal of Clinical Investigation117, 40344043 . doi:10.1172/JCI32994.
Rosengren, A. H., Jokubka, R., et al. Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science327, 217220 . doi: 10.1126/science.1176827.
Winzell, M. S. & Ahren, B. G-protein-coupled receptors and islet function-implications for treatment of type 2 diabetes. Pharmacology and Theraputics116, 437448 . doi:10.1016/j.pharmthera.2007.08.002.
Recommended Reading: Is Honey Better Than Sugar
What Could Go Wrong With The Pancreas
When the cells that make insulin either stop working altogether, or become inefficient and do not make enough insulin, this causes diabetes mellitus’ data-content=’1282′ >diabetes mellitus. Type 1 diabetes mellitus is caused when the body’s immune system attacks its own cells in the islets of Langerhans, meaning that these cells cannot produce insulin.;Type 2 diabetes mellitus is a metabolic disorder where the body is no longer able to produce or respond to insulin.
Some women also get diabetes temporarily when they are pregnant.;This is called gestational diabetes. There are other rarer forms of diabetes, some of which are inherited. In addition, people will get diabetes if their pancreas is taken away surgically or damaged .
Very rarely, patients develop growths of the cells that make up the islets of Langerhans. These may be benign tumours, where a particular kind of cell multiplies and makes large quantities of its hormone whether it is needed or not.;;For example, if the tumour is made of insulin-producing cells, it is called an insulinoma.;This is where too much insulin is produced when it is not required. This also happens with glucagon-producing cells, or a glucagonoma, which produces too much glucagon. These and other hormone-producing tumours in the pancreas are very rare, but endocrinology specialists have important parts to play in diagnosing patients with these tumours and contributing to their management and treatment.;; ;;;;;;;
The Important Roles Of Insulin And Glucagon: Diabetes And Hypoglycemia
The human body wants blood glucose maintained in a very narrow range. Insulin and glucagon are the hormones which make this happen. Both insulin and glucagon are secreted from the pancreas, and thus are referred to as pancreatic endocrine hormones. The picture on the left shows the intimate relationship both insulin and glucagon have to each other. Note that the pancreas serves as the central player in this scheme.; It is the production of insulin and glucagon by the pancreas which ultimately determines if a patient has diabetes, hypoglycemia, or some other sugar problem.
Read Also: What Is The Best Blood Sugar Test Kit
Pathways Involved To Regulate Blood Glucose Levels In Normal And Abnormal Conditions
Pancreas maintains blood glucose levels within a very narrow range through glucagon and insulin by their opposing and balanced actions by the phenomenon of glucose homeostasis. During sleep/between meals/when blood glucose levels are low/during prolonged fasting, -cells release glucagon and promote hepatic glycogenolysis. Along with this, glucagon do hepatic and renal gluconeogenesis and increase endogenous blood glucose levels. In elevated exogenous glucose levels, after a meal, insulin secretion is stimulated from -cells and after docking to its receptor on muscle and adipose tissue, insulin enables insulin-dependent uptake of glucose into tissues and lowers blood glucose levels by removing the exogenous glucose from the blood stream . Moreover insulin enhances glycogenesis, lipogenesis and incorporation of amino acids into proteins; thus it performs its anabolic action as compared to glucagon which is catabolic. Along with pancreas, other organs also regulate blood glucose levels .
Figure 2.
Response To A Decrease In Blood Glucose
Several hours after eating a meal, when the body is in the post-absorptive state, insulin levels fall along with blood glucose and this results in the hormone glucagon being released by the alpha cells of the pancreas.
The role of glucagon – Glucagon has the opposite effect to insulin in that it increases blood-glucose levels and promotes processes that spare glucose utilisation.
Glucagon works primarily on the hepatocytes in the liver to:
– Convert stored glycogen into glucose and release it into the blood;
– Promote gluconeogenesis, the manufacture of new glucose from lactic acid and other metabolites.
Glucagon binds to glucagon receptors, which are part of the G-protein-coupled receptor family. This stimulates a series of linked enzyme reactions, resulting in the activation of glycogen phosphorylase, the enzyme responsible for the mobilisation of glycogen reserves into free glucose. Glucagon release is inhibited by both insulin and somatostatin.
Recommended Reading: What Artificial Sweetener Tastes The Most Like Sugar
How Is Glucagon Controlled
Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels.;Glucagon is released to stop blood sugar levels dropping too low , while insulin is released to stop blood sugar levels rising too high .;
The release of glucagon is stimulated by low blood glucose, protein-rich meals and adrenaline . The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
In the longer-term, glucagon is crucial to the bodys response to lack of food.;For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose.
Ideal Blood Sugar Levels
A range of factors, including insulin resistance, diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
The standard measurement units for blood sugar levels are milligrams per deciliter . Ideal blood sugar ranges are as follows:
| Timing |
Insulin and glucagon do not take immediate effect, particularly in people whose blood sugar levels are extremely high or low.
Also Check: How Do You Test Your Blood Sugar
The Role Of Glucagon In Blood Glucose Control
The effect of glucagon is to make the liver release the glucose it has stored in its cells into the bloodstream, with the net effect of increasing blood glucose. Glucagon also induces the liver to make glucose out of building blocks obtained from other nutrients found in the body .
Our bodies desire blood glucose to be maintained between 70 mg/dl and 110 mg/dl . Below 70 is termed “hypoglycemia.” Above 110 can be normal if you have eaten within 2 to 3 hours.; That is why your doctor wants to measure your blood glucose while you are fasting…it should be between 70 and 110.; Even after you have eaten, however, your glucose should be below 180. Above 180 is termed “hyperglycemia” . If your 2 two blood sugar measurements above 200 after drinking a sugar-water drink , then you are diagnosed with diabetes.;;
How Can Chemicals Affect The Endocrine System
Scientific research on human epidemiology, laboratory animals, and fish and wildlife suggests;that environmental contaminants can disrupt the endocrine system leading to adverse-health consequences. It is important to gain a better understanding of what concentrations of chemicals found in the environment may cause an adverse effect.;Various types of scientific studies are necessary to resolve many of the scientific questions and uncertainty surrounding the endocrine disruptor issue. Many such studies are currently underway by government agencies, industry, and academia.
Learn more with EDSP about concerns and examples of;endocrine disruption.
Read Also: Does Wine Lower Blood Sugar